Major depressive disorder (MDD) is ranked second among all diseases in global impact. Unfortunately, many patients have treatment-resistant MDD (TRD), for which the most effective antidepressant treatment option is electroconvulsive therapy (ECT). However, the neurocognitive adverse effects (e.g., anterograde and retrograde amnesia) induced by ECT mitigate the attainment of desired clinical outcomes. As such, the development of new and safe neuromodulatory antidepressant interventions is strongly warranted. One new type of neuromodulation treatment that has antidepressant properties and is under active development is magnetic seizure therapy (MST). MST is neurocognitively safer than ECT because it uses magnetic rather than electrical fields to induce seizures, which have shallower penetration and therefore avoid the undesired side-effect of delivering intense electrical stimulation to the medial temporal lobe. As yet there has been no research into the neuromechanisms underlying MST’s antidepressant and neurocognitive effects. To systematically uncover these mechanisms, we are building upon an international, NIMH funded (R01 MH112815), US Food and Drug Administration Investigational Device Exemption (IDE; #G170127) approved clinical study that will compare and contrast clinical and neurocognitive outcomes of ECT and MST. The goal of this R01 is to conduct research Ascertaining Neurocircuitry to Enhance Neuromodulation Development (ASCEND). In the proposed study, we will capitalize on that project by adding advanced magnetic resonance imaging (MRI), individualized 3-D computational head modeling of ECT and MST (E-fields in stimulated brain regions), and neurophysiological modeling of activity propagation and plasticity resulting from each treatment type. This innovative 5-year project has two aims: 1) Determine the common and distinct neural circuit correlates of antidepressant treatment response between RUL-UB-ECT and MST, and 2) Determine the common and distinct neural circuit correlates of memory side effects between RUL-UB-ECT and MST. The proposed study will draw upon an interdisciplinary team from diverse backgrounds including translational neurocognitive science, neuropsychology, computational neuroscience, psychiatry, neuroimaging, bioengineering, and biostatistics. The synthesis of physical (E-field) and physiological (neural activity and dynamics) computational modeling and MRI with the clinical and neurocognitive metrics from the current NIMH-funded clinical trial will allow us to determine neuromodulation-induced changes in neurocircuitry, and their corresponding relationships to behavior. Such knowledge will elucidate the neural mechanisms of antidepressant seizure therapy (ECT, MST) to inform new treatment methods that optimally target neurocircuitry related to symptom improvement, while ensuring neurocognitive safety. These developments will make a major contribution to improving the lives of the many patients with TRD and yield a substantial positive public health impact.
The Confirmatory Efficacy and Safety Trial of Magnetic Seizure Therapy for Depression (CREST-MST) Trial aims to assess the efficacy and tolerability of MST as an alternative to ECT for depression. A clinical specialist trained in MST uses a magnetic coil fit to the individual patient to stimulate therapeutic seizures in the patient’s brain. The seizure activity increases blood flow to the areas where depression originates, which might help reduce symptoms of depression. Magnetic currents do not penetrate as deeply as the electrical currents used in electroconvulsive therapy and can be focused more precisely, which may result in a relatively better cognitive safety profile. Study activities take place in our state-of-the-art psychiatry space at Clements University Hospital and are fully integrated into the UTSW interventional psychiatry service.
This study uses MRI scans and clinical and cognitive tests to evaluate optimal ECT dosing. For this research you would be asked to complete cognitive tasks, mood scales, and MRI scans at three time points during your medically indicated ECT treatment. The three research visits are before starting ECT, midway through, and at the end of ECT treatment. You would also complete a research follow-up visit 1-month after ending ECT.
The purpose of the study is to evaluate the clinical efficacy and safety of SCC DBS for TRD. An innovative method for the definition of DBS target will be applied that redefines the concept of targeting as one of targeting a symptomatic network rather than a structural brain region using subject-based brain anatomy to define the target location. The correlation between imaging findings at baseline with the mood score changes at different time points of the study will be investigated.
This clinical trial involves 12-months open-label bilateral DBS that targets SCC in subjects with TRD. Following open label optimization, to control for possible placebo, each subject will enter a 6-month double blinded randomized discontinuation, intended to confirm clinical benefit of DBS among responders.
The total duration of the study will be approximately four years and eight months.
The purpose of the study is to evaluate the safety and effectiveness of Deep Brain Stimulations (DBS) in the treatment of schizophrenia. Our overall objective is to use next generation DBS combined with antecedent stereo electroencephalography (sEEG) mapping to establish a novel therapy for schizophrenia given the limitations of current treatment modalities.
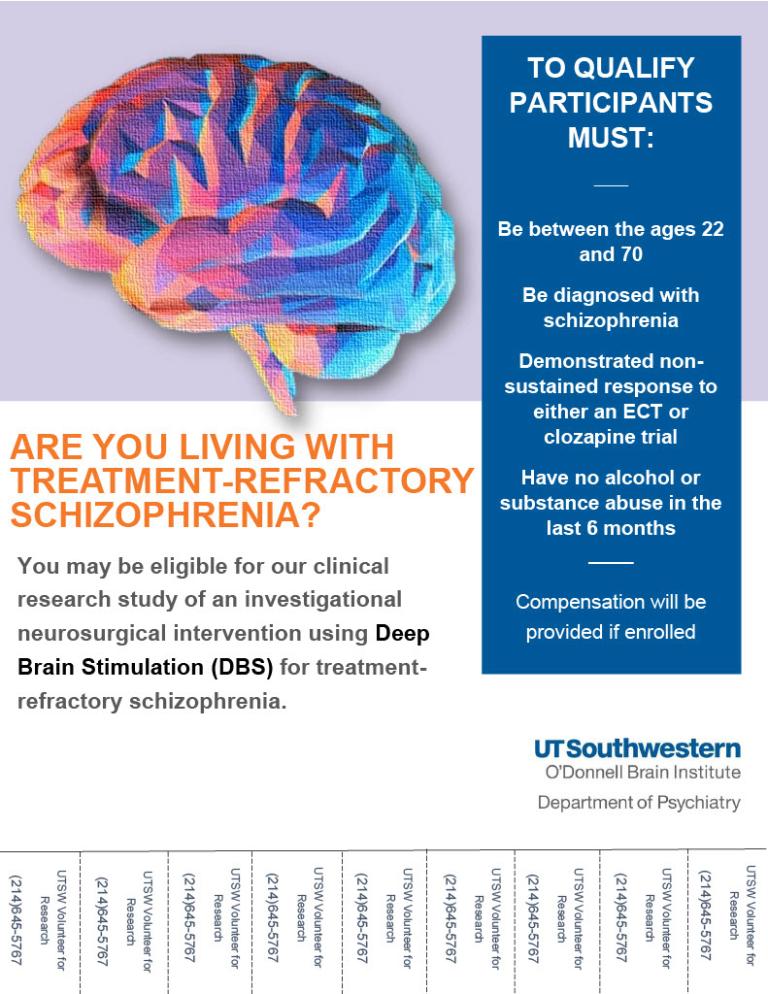 DBS - Psychosis Flyer
DBS - Psychosis Flyer This is a cross-sectional pilot study designed to establish hot and cold cognitive functions and underlying neurocircuitry in older adults with MDD. The investigators will study 60 participants aged 21-80 years old with MDD. All participants will undergo clinical and neurocognitive assessment, and Magnetoencephalography (MEG)/Magnetic resonance imaging (MRI) procedures at one time point. The investigators will also enroll 60 demographically matched comparable, never-depressed healthy participants (controls) to establish cognitive benchmarks. Healthy controls will complete clinical and neurocognitive measures at one time point. To attain a balanced sample of adults across the lifespan, the investigators will enroll participants such that each age epoch (e.g., 21-30, 31-40, etc.) has a total of ten subjects (n=10) in both the healthy control cohort and depressed cohort.
This research study investigates the genetic factors that contribute to mood disorders, specifically major depressive disorder and bipolar disorder. This study also explores how genetic factors contribute to a patient’s response to Electroconvulsive Therapy (ECT). This study is supported by the National Institute of Mental Health. It is being done to increase the body of knowledge of the genetic factors that contribute to mood disorders, knowledge that will help predict whether an individual is likely to be a good candidate for ECT.
This Randomized Control Trial is a blinded, randomized, multicenter controlled study intended to collect evidence that VNS Therapy as an adjunctive therapy improves health outcomes for patients with TRD. The study is intended to demonstrate that VNS Therapy treatment is reasonable and necessary to treat Medicare beneficiaries with TRD by providing sufficient evidence to conclude that VNS Therapy improves key health outcomes (rate of, time to and duration of response and remission, disability, quality of life, general psychiatric status and suicidality) while minimizing potential harms.
Currently, enrollment in this study is the only coverage pathway available for Medicare beneficiaries with TRD to access VNS Therapy.
Subjects will participate in the RCT for approximately 12 months post device activation visit, after which they will be followed for an additional 4 years of study participation (“Follow-up”).
Many people have severe depression, bipolar disorder, or other serious mental illnesses that don’t respond to medication or psychotherapy.
As part of one of the largest psychiatry programs in the country, UT Southwestern Medical Center’s specialists offer electroconvulsive therapy (ECT), a safe, effective treatment that can help manage symptoms.
UT Southwestern Medical Center is home to one of the premier centers in the world for the diagnosis and treatment of mental illness. The faculty at the Multispecialty Psychiatric Clinic offers an extensive range of top-quality mental health services in an outpatient setting. Our services are delivered in comfortable, private offices and are provided by caring board-certified psychiatrists and psychologists.
The Doctoral Program in Clinical Psychology at UT Southwestern Medical Center is an American Psychological Association-accredited training program that prepares skilled psychologists to serve as clinicians as well as researchers. The Program includes an exclusively affiliated, and separately APA-accredited, doctoral internship in clinical psychology.
The Doctoral Program’s basic training philosophy reflects a clinician-researcher model of training that prepares individuals for the practice of clinical psychology, broadly conceived. The combined experience of clinical and research settings reflects the Program’s clinician-researcher philosophy. The Clinical Psychology Program’s model provides research training that equips students pursuing more clinically oriented careers with the skills to critically evaluate scientific material. Students pursuing academic or research careers have a solid clinical foundation to build on.